Ebstein's Anomaly With Right Atrial Thrombus in 23 Years Old Man at Reference National Teaching Hospital of Ndjamena: A Case Report.
Abstract
Ebstein’s anomaly is a rare congenital heart disease. It is usually associated with other congenital defects, particularly atrial septal defect/patent foramen ovale (PFO). We report here the case of Ebstein's disease revealed in a 23-year-old adult admitted for palpitations and exertional dyspnoea. He was in heart failure. The EKG showed atrial flutter . Cardiomegaly was present with a cardiothoracic index of 0.7. On echocardiography, the apical displacement of the tricuspid septal leaflet was 15 mm/m2 , the Celermajer index was Grade 3. There was a large thrombus floating in the right atrium. While awaiting surgical management, the patient was being treated with diuretics, digitalis and anticoagulants.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2024 Oumar Mahamat -Azaki, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have no conflict of interest to declare related to the manuscript.
Citation:
Introduction
Ebstein anomaly (EA) was first described by Wilhelm Ebstein in 1866 in an autopsy specimen, first clinically characterized in 1947 by Helen Taussig, and first diagnosed in a live patient in 1949 1. Ebstein anomaly (EA) is among the rarest congenital cardiac malformations, with a prevalence of 4.4 per 100,000 live births 1. It is a malformation of the tricuspid valve (TV) with myopathy of the right ventricle (RV) that has variable presentation of the anatomic and pathophysiologic characteristics. Anatomical features include : (1) failure of TV leaflet delamination, (2) apical descent of the functional tricuspid orifice, (3) right ventricular dilation and “atrialization,” (4) anterior leaflet abnormal fenestrations and tethering, and (5) right atrioventricular junction dilation. The critical distinguishing feature of EA from other congenital regurgitant lesions is the degree of apical displacement of the septal leaflet (≥ 8 mm/m2 body surface area) 2. Ebstein anomaly is a spectrum of tricuspid valvular (TV) and right ventricular (RV) dysplasia. Morbidity and mortality are thought to be related to the degree of TV regurgitation, the size, thickness, and function of the RV, and the presence or absence of an atrial septal defect (ASD). Patients with mild forms of Ebstein anomaly may live normal life-spans, but many will require surgery 3. Arrhythmias are the most common presenting feature of Ebstein patients in adulthood and are poorly tolerated 4 . Accordingly, management of EA ranges from no treatment in asymptomatic patients with isolated mild apical displacement to medical and surgical palliation in patients with severe displacement. Treatment of significant forms of EA is surgical, with valve-sparing surgery preferred. A revolution in the treatment of EA came with the technique of cone tricuspid valve reconstruction according to Da Silva; the procedure can be performed with very low morbidity and mortality rates4. We report here the first case of Ebstein's disease in Chad.
Patient’s identification and medical history
M.Z.I 23 years old male with no previous history was seen for NYHA II dyspnoea progressing to NYHA III associated to lightheadedness, fatigue and palpitations that had been evolving for six months. The palpitations were intermittent, with a regular rhythm and abrupt onset and cessation, and the patient had not reported any triggering, stimulating or calming factors. He had no chest pain, lower limb oedema or other associated functional signs. When these symptoms persisted, the patient consulted a primary health centre, a chest X-ray was requested showing cardiomegaly, he was referred to the Reference National Teaching Hospital of Ndjamena in cardiology department for further investigations and management.
Clinical findings
In general, the patient was conscious, eupneic at rest with a respiratory rate 18 cycles/minute, acyanotic with SaO2= 96% on room air, and normo-coloured conjunctivae. His weight was 50 kg, his height 170 cm, his blood pressure 100/85 mmHg symmetrically across the 2 upper limbs, heart rate 120 beats/min.
Physical examination revealed signs of right heart failure: the jugular vein was elevated, the hepatomegaly was tender with a smooth surface and a firm lower border with hepatojugular reflux. Cardiovascular auscultation revealed regular, rapid sounds with no additional sounds. Chest and other systemic examinations were unremarkable.
Diagnostic approach
The frontal chest X-ray showed cardiomegaly with a cardiothoracic index of 0.7. The thoracic cavity and pulmonary parenchyma were without abnormality (Figure 1).
Figure 1.Frontal chest radiograph showing cardiomegaly
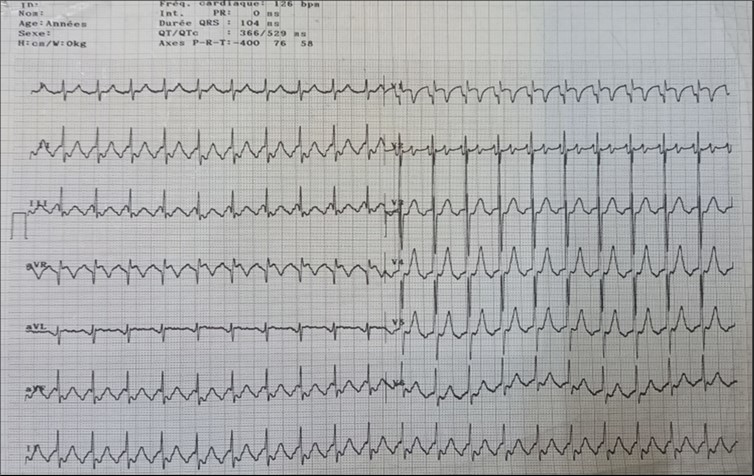
The EKG showed atrial flutter (Figure 2 ).
The patient underwent echocardiography (Figure 3 ) showing a low insertion of the septal and posterior leaflets of the tricuspid valve 22 mm below the tricuspid annulus, the anterior leaflet having reduced reduced mobility. Significant dilatation of the the right atrium by atrialisation of the right ventricle (RV). The rudimentary RV and its atrial stump are dilated and responsible for compression of the LV. There was no tricuspid insufficiency. No other associated congenital anomaly. However, we found a large floating thrombus in the right atrium measuring 64 mm x 30 mm in diameter. This was therefore Ebstein's disease at stage C of the Carpentier classification. The apical displacement of the tricuspid septal valve was 22 mm or 15 mm/m2). The surface area of the atrium and the atrialized right ventricle was 45 cm2 , the surface area of the right ventricle and the left cavities was 30 cm2 , the Celermajer index was calculated at 1.4 ( Grade 3).
Figure 3.Transthoracic echocardiography, apical four chambers view . Apical displacement of the tricuspid valve (a) and right atrial thrombus (b).
Laboratory findings
Biological tests, including blood count, renal, liver and haemostasis tests, were unremarkable.except for hypokalemia at 3 mEq/L.
Therapeutic intervention and fellow up
Routine follow-up with an adult congenital cardiologist is recommended for all patients with EA regardless of disease severity. Frequency of follow-up depends on the patient specific anatomic, physiologic, and clinic characteristics, and ranges from every 1–2 years to every 6 months.
He has treated with Furosemide 40 mg daily, digitalis and anticoagulants. The evolution was marked by regression of heart failure symptoms. Our patient was eligible for surgery, which had to be performed abroad due to lack of adequate resources. Assessment of arrhythmias, progressive RV enlargement, and/or systolic function deterioration of the RV should be closely followed. we examine him every 3 months.
Patient consent and adherence to institutional guidelines
Informed consent was obtained from the patient before the scan was carried out.
Discussion
Ebstein’s disease is a rare congenital heart disease. It is an isolated condition that remains largely undetected in childhood 5. This was the case in our study, the four patients were adolescents. The natural history of Ebstein’s disease is difficult to understand in a simple way because of the wide spectrum of clinical presentation it offers: incidental discovery in the fetus during per-partum ultrasound, cyanosis in the newborn, heart failure in the infant, heart murmur in the child and rhythm disorders in the adolescent and adult 6. Our patient is in right heart failure . The main hemodynamic abnormality producing symptoms in Ebstein’s malformation is tricuspid regurgitation. Symptoms are generally related to the degree of the regurgitation. Cyanosis is due to right to left shunting through an interatrial communication (patent foramen ovale or atrial septal defect). Symptoms vary markedly, as would be expected from the large anatomic spectrum of alterations. Although symptoms are lacking in a few patients, cyanosis and dyspnea are present in the majority 7.
Cardiomegaly is frequent in Ebstein’s anomaly. A cardiothoracic ratio of at least 0.65 is associated with a poor prognosis 8 . This was the case with our patient.
The pathologic abnormalities in EA, including a markedly enlarged right atrium and right ventricle as well as associated atrioventricular (AV) accessory conduction pathways (APs), provide the substrate for the development of both supraventricular and ventricular tachyarrhythmias 9 The electrocardiogram in Ebstein’s anomaly is often abnormal. It may show right ventricular hypertrophy, first-degree atrioventricular block, and right bundle branch block 10
The ECG abnormalitie found in our patient was atrial flutter. The patients with atrial flutter may be at an increased risk of a stroke compared with the general population because during atrial flutter blood may not move as rapidly through the upper heart chambers (the atria) as it does during normal sinus rhythm. Slower movement of the blood carries the risk of formation of small blood clots that can cause a stroke. The risk of stroke is not the same for all people with atrial flutter. Therefore, some people with atrial flutter may require treatment with a blood thinner called warfarin to reduce the risk of stroke 10
Echocardiography is an essential diagnostic test and allows accurate assessment of the tricuspid valve leaflets and the size and function of the heart chambers. The main feature of Ebstein’s anomaly is an apical displacement of the tricuspid septal leaflet of at least 8 mm/m2. The average displacement in our patient was 15 mm/m2
In 1988, Carpentier et al proposed the following classification of Ebstein’s anomaly: type A, the volume of the true right ventricle is adequate; type B, a large atrialized component of the right ventricle exists, but the anterior leaflet of the tricuspid valve moves freely; type C, the anterior leaflet is severely restricted in its movement and may cause significant obstruction of the right ventricular outflow tract; and type D, almost complete atrialization of the ventricle except for a small infundibular component 8, 11.
Celermajer et al described an echocardiographic grading score for neonates with Ebstein’s anomaly, extended Glasgow Outcome Scale, with grades 1 to 4. The ratio of the combined area of the right atrium and atrialized right ventricle is compared with that of the functional right ventricle and left heart (ratio <0.5, grade 1; ratio of 0.5 to 0.99, grade 2; ratio of 1.0 to 1.49, grade 3; ratio ≥1.5, grade 4) 8, 11.
An atrial septal defect is present in more than one-third of hearts, and most of the remainder have a patent foramen ovale accounting for the right-to-left shunt. An intact atrial septum is rare and usually seen in adults 7.
In our case, the patient had, type C of EA and Grade 2. The investigation also revealed a large thrombus floating in the right atrium and no obvious regurgitation of the tricuspid valve. In addition, the septa was intact, there was no persistence of the ductus arteriosus, the pulmonary and aortic pathway were unobstructed.
The management of Ebstein’s anomaly varies according to anatomical form and clinical presentation. Surgical intervention is indicated when the patient becomes symptomatic (NYHA III-IV) or when arrhythmia or increased cardiomegaly occur, or when echocardiographic changes such as deterioration of right ventricular function or worsening of the echographic severity index grade occur 12. It consists of reconstruction with or without an upper cavo-pulmonary bypass or tricuspid valve replacement or the cone technique. Our patient has a surgical indication. Electrophysiologic testing plays an important role in the diagnosis and management of patients with EA and supraventricular tachyarrhythmias. Therefore all patients with documented tachycardia or a history of palpitations should undergo preoperative electrophysiologic testing regardless of evidence of preexcitation. Because the late success rate for catheter ablation of accessory conduction pathways (APs) in EA is suboptimal, we favor primary reliance on surgical ablation. Concomitant arrhythmia procedures can be combined with EA corrective surgery without increase in early mortality; we conclude they should be added to EA repairs for all patients who have supraventricular tachyarrhythmias 9.
Conclusions
Our case highlights a rare form of Ebstein's disease with a large right intra-atrial thombus. It is a rare disease discovered late in adulthood with no vicarious shunt. Echocardiography is used to establish the diagnosis and to assess its severity. Ebstein's anomaly is tricuspid valve and right ventricular malformation with variability in anatomy, pathophysiology, and clinical presentation which cannot be managed surgically in our resource-limited setting. The great anatomical heterogeneity of EA generates a wide spectrum of clinical features at presentation which cannot be managed surgically in our context of limited resources. Hence the importance of antenatal ultrasound diagnosis with a view to possible termination of pregnancy.
References
- 2.Holst K A, Connolly H M, Dearani J A. (2019) Ebstein’s Anomaly. Methodist DeBakey Cardiovascular Journal. 15-138.
- 3.Functional Status After Operation for Ebstein Anomaly n.d. https://doi.org/10.1016/j.jacc.2008.03.064
- 4.Celermajer D S, Bull C, Till J A, Cullen S, Vassillikos V P et al. (1994) Ebstein’s anomaly: Presentation and outcome from fetus to adult. , Journal of the American College of Cardiology 23, 170-6.
- 5.Gupta S, Naik R, Hafiz M, Choudhary N. (2020) Case report: An uncommon association of Ebstein’s anomaly and rheumatic mitral stenosis. IHJ Cardiovascular Case Reports (CVCR). 4-41.
- 6.Hadraoui H E, Barkat A. (2016) Maladie d’Ebstein révélée par une anasarque fœtoplacentaire: à propos d’une observation originale. Pan Afr Med J. 24. https://doi.org/10.11604/pamj.2016.24.279.9970
- 7.Frescura C, Angelini A, Daliento L, Thiene G. (2000) Morphological Aspects of Ebstein’s Anomaly in Adults. Thorac Cardiovasc Surg. 48-203.
- 8.Sainathan S, LDFD Silva, JPD Silva. (2020) Ebstein’s anomaly: contemporary management strategies. , J Thorac Dis 1161-73.
- 9.Khositseth A, Danielson G K, Dearani J A, Munger T M, Porter C J. (2004) Supraventricular tachyarrhythmias in Ebstein anomaly: Management and outcome. The Journal of Thoracic and Cardiovascular Surgery 128-826.
- 10.Kumar P, Singhal G, Sinha S, Pandey U, Thakur R et al. (2015) Ebstein Anomaly With Right Atrial Clot. Cardiol Res. 319-23.