Diagnostic Performance of Smear Microscopy and Xpert MTB/RIF Versus MGIT Culture in Republic of Congo
Abstract
In the Republic of the Congo, tuberculosis (TB) remains a major public health concern. Although the GeneXpert MTB/RIF assay is the WHO-recommended first-line diagnostic test, smear microscopy is still used for treatment monitoring and in facilities where molecular testing is limited. Evaluating the diagnostic accuracy of smear microscopy compared to GeneXpert and MGIT culture is essential to guide diagnostic strategies and strengthen TB control in the country. A cross-sectional study was conducted among 92 presumptive pulmonary TB patients at Makelekele Hospital. Sputum samples were analyzed by smear microscopy, GeneXpert MTB/RIF, and MGIT culture. Sensitivity, specificity, positive and negative predictive value were calculated for smear microscopy and GeneXpert, using culture as the reference standard. Culture detected more Mycobacterium tuberculosis than microscopy (49% vs. 32%, P<0.001). Smear microscopy showed a sensitivity of 58% (95% CI: 43–71%) and specificity of 92% (95% CI: 80–97%). GeneXpert detected more MTB (62% vs. 49%, P<0.001) with a sensitivity of 98% (95% CI: 89–100%) and specificity of 72% (95% CI: 58–83%). GeneXpert showed superior sensitivity for TB detection, while microscopy remained specific. Expanding GeneXpert testing across the Republic of the Congo will improve TB management.
Author Contributions
Academic Editor: N. R. Rajagopalan, Assistant Professor, Department of Chemistry, St. Joseph’s College of Engineering, Chennai
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2025 Darrel Ornelle Elion Assiana, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have no conflict of interest to declare.
Citation:
Introduction
Tuberculosis (TB) remains one of the major infectious diseases worldwide, representing a significant public health problem, particularly in sub-Saharan Africa 1, 2. According to the latest World Health Organization, 2024 report, approximately 10.8 million people developed TB in 2023, with 1.25 million deaths, including a substantial proportion among people living with HIV 1. Early and accurate detection of Mycobacterium tuberculosis (MTB) is crucial to reduce TB-related morbidity and mortality. Diagnostic methods in use include smear microscopy, molecular tests such as Xpert MTB/RIF, and culture, which is considered the gold standard due to its high sensitivity and ability to provide a definitive diagnosis 3, 4.
For decades, direct smear microscopy has been the most widely available initial diagnostic test in resource-limited settings such as the Republic of Congo 5. In this country, TB is also a major concern, with cases of multidrug-resistant TB (MDR-TB) and frequent HIV co-infections, complicating disease management and control 6, 7. While its technical simplicity and low cost are operational advantages, its notoriously low sensitivity, particularly in HIV patients or those with paucibacillary disease, likely results in a substantial number of missed diagnoses 8. However, the technical complexity, long turnaround time, and biosafety requirements of culture limit its utility for rapid clinical decision-making at the point of care 3.
To bridge this diagnostic gap, the WHO recommends the Xpert MTB/RIF assay as the initial diagnostic test for TB because of its ability to rapidly detect MTB complex DNA and rifampicin resistance 4, 9. In the Republic of Congo, this recommendation has driven a significant shift in diagnostic policy, with Xpert now widely adopted as the first-line diagnostic tool in more than 40% of testing centers 7.
However, critical reliance on microscopy persists for patient follow-up to monitor treatment response, even in centers equipped with GeneXpert. Moreover, in many centers, microscopy remains the only on-site tool for both initial diagnosis and follow-up. This continued, widespread reliance on direct smear microscopy for both initial diagnosis and treatment monitoring underscores the need for a contemporary evaluation of its performance in the Congolese context, especially in high-risk populations such as people living with HIV 5, 6, 10. Generating such local evidence is essential to validate current practices, identify potential risks, and guide the evolution of national TB diagnostic strategies.
Methodology
Ethical Approval
The study protocol was approved by the Institutional Ethics Committee of the Congolese Foundation for Medical Research (015/CIE/FCRM/May 30, 2018). All procedures were conducted in accordance with the Declaration of Helsinki and national ethical guidelines. Written informed consent was obtained from adult participants, while assent from minors was obtained along with consent from their legal guardians.
Type and population of study
This is a cross-sectional study, conducted from October 2018 to October 2019 and targeted presumptive pulmonary tuberculosis participants and who had never received treatment recruited. Eligible participants were between 8 and 70 years of age, presenting TB clinical signs, without prior anti-TB treatment, voluntarily consented and assented to HIV testing, and residing in Brazzaville during the study period. Participants with diseases such as cancer, advanced HIV-AIDS, severe malaria and extra-pulmonary TB were excluded.
Sample Collection and study design
The study design was based on a previously published survey conducted among the same group of presumptive TB patients 6. From October 2018 to October 2019, sputum samples were collected from patients with presumed pulmonary tuberculosis hospitalized at the Makelekele Hospital located in Brazzaville, Republic of Congo. Sociodemographic, behavioral, and clinical data were recorded using a standardized, structured questionnaire.
After informed consent was obtained, a 5 mL blood sample was taken for HIV screening, preceded by a pre-test interview for HIV. Two sputum samples of 3 mL each were collected according to national guidelines: a single sample on the first day in the hospital and a morning sample on the second day at home, sent the same day to the mycobacteria laboratory at Makélékélé Reference Hospital.
All samples were transported at 4–8°C to the mycobacteria laboratory at the Christophe Mérieux Center for Research on Infectious Diseases (CeRMI-CM). Sputum samples were decontaminated using the BD BBL® MycoPrep™ kit before being cultured (Figure 1).
Blood was used for HIV screening, while sputum was analyzed for Mycobacterium tuberculosis detection using microscopy (Ziehl–Neelsen staining), Xpert MTB/RIF test (GeneXpert Cepheid), and culture in MGIT BACTEC 960 liquid medium 2, 8, 12, 11.
Figure 1.Flowchart of patient recruitment at Makelekele Referral Hospital and laboratory methods used.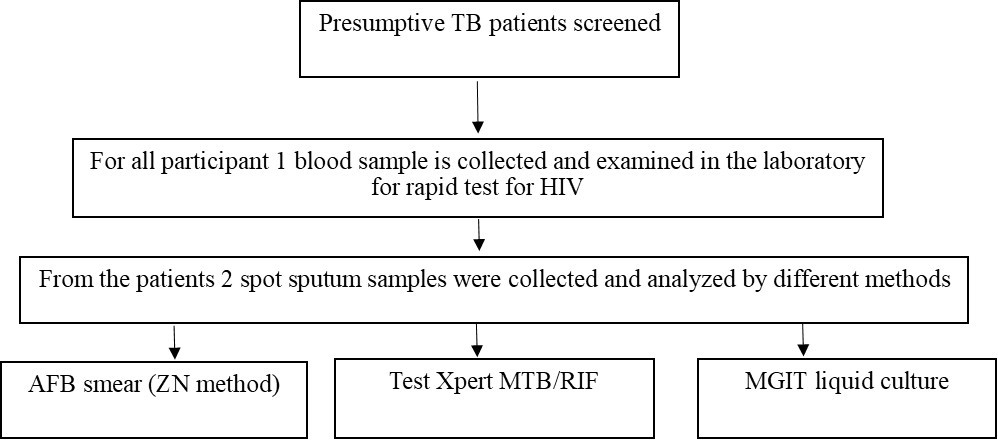
Mycobacterial Culture
Decontaminated sputum samples were inoculated into BACTEC MGIT 960 culture tubes (Becton Dickinson, United States of America) supplemented with oleic acid, albumin, dextrose, and catalase, together with polymyxin B, amphotericin B, nalidixic acid, trimethoprim, and azlocillin as antimicrobial agents 11, 13. The tubes were incubated in the MGIT 960 system 11. Positive cultures were confirmed by Ziehl–Neelsen staining and checked for sterility on blood agar 8. Cultures were considered negative after forty-two days without growth 3, 11.
Statistical analysis
Participant characteristics were summarized using standard descriptive statistics. Graph Pad Prism (Version 8.0.2) was used for statistical analyses. The count data were expressed as rate (%), Fisher. Two-sided test, P value <0.05 indicated a statistically significant difference. Microscopy and GeneXpert sensitivity and specificity to detect MTB in sputum were determined using following formula. Sensitivity = true positive / (true positive + false negative) × 100% Specificity = true negative / (true negative + false positive) × 100% PPV = true positive / (true positive + false positive) × 100% NPV = true negative / (true negative + false negative) × 100%.
Results
Sociodemographic, clinical, risk behavior, and comorbidity characteristics of patients enrolled in the study
A total of 92 patients were included in the study. The gender distribution was balanced, with 47 women (51.1%) and 45 men (48.9%). The mean age of the participant was 38.2 ±15 years. Most were in the 18–44 years age group (55.4%), followed by those aged ≥45 years (35.9%) and under 18 years (8.7%). Regarding marital status, single patients predominated. In addition, a large proportion of participants had secondary or higher education. Concerning risk behaviors, 43 patients (46.7%) reported alcohol consumption, 20 (21.7%) reported tobacco use, and 5 (5.4%) reported cannabis use. Twenty-two patients (23.9%) were HIV-positive, while 70 (76.1%) were HIV-negative. The dominant clinical signs included: chronic cough in 66 cases (71.7%), acute cough in 28 (30.4%), fever in 72 (78.3%), weight loss in 82 (89.1%), physical asthenia in 27 (29.3%), and anorexia in 19 (20.7%), as shown in Table 1.
Table 1. Sociodemographic, clinical, risk behavior, and comorbidity characteristics of patients enrolled in the study.| Characteristics | Number of patients (n=92) | Percentage (%) |
|---|---|---|
| Sociodemographic | ||
| Age group (years) | ||
| <18 | 8 | 8.7 |
| 18–44 | 51 | 55.4 |
| ≥45 | 33 | 35.9 |
| Median age | 38.2 | |
| Interquartile range | 23.0-49.7 | |
| Gender | ||
| Female | 47 | 51.1 |
| Male | 45 | 48.9 |
| Marital status | ||
| Single | 81 | 88.0 |
| Cohabiting | 11 | 12.0 |
| Education level | ||
| None / Primary | 16 | 17.4 |
| Secondary / Higher | 76 | 82.6 |
| Season of recruitment | ||
| Rainy season | 57 | 62.0 |
| Dry season | 35 | 38.0 |
| Tuberculosis risk behaviors | ||
| Alcohol use | 43 | 46.7 |
| Tobacco use | 20 | 21.7 |
| Cannabis use | 05 | 05.4 |
| HIV comorbidity | ||
| Negative | 70 | 76.1 |
| Positive | 22 | 23.9 |
| Clinical signs | ||
| Chronic cough | 66 | 71.7 |
| Acute cough | 28 | 30.4 |
| Fever | 72 | 78.3 |
| Anemia | 10 | 10.9 |
| Neurological signs | 04 | 04.3 |
| Night sweats | 15 | 16.3 |
| Physical asthenia | 27 | 29.3 |
| Anorexia | 19 | 20.7 |
| Weight loss | 82 | 89.1 |
Performance of microscopy in TB diagnosis using culture as the gold standard
The performance of smear microscopy for the detection of pulmonary TB was evaluated using culture as the gold standard (Table 2).
Table 2. Performance parameters of MTB detection microscopy compared to the culture| Culture | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | |||
| Positive | Negative | ||||||
| Microscopy | Positive | 26 | 4 | 58(43.3–71) | 91.5(80.1–96.6) | 86.7(70.3–94.7) | 70(58–79.4) |
| Negative | 19 | 43 | |||||
Compared to the culture, smear microscopy showed a lower rate of MTB detection (P<0.001) (49% vs 32%). Considering culture as the gold standard, smear microscopy demonstrated a sensitivity of 57.8% (95% CI: 43.3–71.0%) and a specificity of 91.5% (95% CI: 80.1–96.6%). The positive predictive value was 86.7% (95% CI: 70.3–94.7%), and the negative predictive value was 69.4% (95% CI: 57.0–79.4%). The Fisher’s exact test showed a statistically significant association between microscopy and culture results (Fisher’s exact test, p < 0.0001, two-sided).
Performance of Xpert MTB/RIF for TB diagnosis using culture as the gold standard
The performance of Xpert MTB/RIF was also assed using culture as the gold standard (Table 3).
Table 3. Performance parameters of MTB detection Xpert MTB/RIF compared to the culture.| Culture | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | |||
| Positive | Negative | ||||||
| Xpert MTB/RIF | Positive | 44 | 13 | 97.8(88.4–99.9) | 72.3(58.1–83) | 77.1(64.7–86) | 97.1(85.4–99.8). |
| Negative | 1 | 34 | |||||
In contrast to microscopy Xpert MTB/RIF detected more MTB cases than culture (62% vs 49%, p < 0.001). Using culture as the reference, Xpert MTB/RIF demonstrated a sensitivity of 97.8% (95% CI: 88.4–99.9%) and a specificity of 77.2% (95% CI: 58.2–83.1%). The positive predictive value was 77.2% (95% CI: 64.8–86.2%), and the negative predictive value was 97.1% (95% CI: 85.5–99.9%). The association between GeneXpert and culture results was also statistically significant (Fisher’s exact test, p < 0.0001, two-sided).
Discussion
This study evaluated the diagnostic performance of Xpert MTB/RIF assay and smear microscopy in a cohort of Congolese patients with presumptive pulmonary tuberculosis hospitalized at the Makelekele Hospital, using culture as the gold standard. Our patient demographic, predominantly younger adults, reflects the typical population most affected by TB 1, 14, 15. Clinically, the same observation was made regarding common symptoms such as chronic cough, HIV infection, and fever 16, 17, 7. The overall findings confirm that while smear microscopy remains highly specific, its sensitivity is considerably lower than that of Xpert MTB/RIF, underscoring the limitation of microscopy as a primary diagnostic tool 18, 2.
Smear microscopy detected fewer MTB cases than culture (32% vs 49%), with a sensitivity of only 57.8%. This means that over 40% of true TB cases confirmed by culture were missed by microscopy. The low sensitivity directly translates into a modest Negative Predictive Value (NPV) of 69.4%, which is a critical weakness in high-burden settings such as the Republic of Congo. This modest NPV indicates that if diagnosis relies solely on microscopy, a substantial proportion of true TB cases may be missed. The finding underlines the limited reliability of smear microscopy in high-burden settings, particularly where early and accurate detection is essential for reducing transmission 19, 2.
In contrast, the Xpert MTB/RIF assay demonstrates a markedly improved diagnostic profile. Xpert MTB/RIF detected more MTB cases than culture (62% vs 49%) and achieved excellent sensitivity (97.8%) while maintaining a high specificity (77.2%). The high negative predictive value (97.1%) suggests that Xpert MTB/RIF is highly reliable in excluding TB in negative cases, a critical advantage in clinical practice. The apparent higher detection rate compared with culture may be due to the molecular assay’s ability to detect DNA from non-viable bacilli or culture losses due to sample degradation or contamination. Despite this, the strong statistical association between Xpert MTB/RIF and culture results supports its validity as a diagnostic tool 20.
The relatively low sensitivity of microscopy observed in our study compared to Xpert MTB/RIF is consistent with several previous studies. Steingart et al. 8, 21 showed that the sensitivity of Ziehl–Neelsen smear microscopy for the detection of MTB ranges between 50% and 60%, whereas the sensitivity of Xpert MTB/RIF can exceed 90%, particularly among HIV co-infected patients. This highlights the limitation of microscopy in detecting paucibacillary cases, which may go unnoticed, while Xpert MTB/RIF, based on PCR amplification, efficiently detects MTB genetic material even at low bacillary loads 12, 22, 23, 9.
Taken together, these findings reinforce the WHO recommendation that Xpert MTB/RIF should be prioritized as the initial diagnostic test for TB 6, 24, especially in high TB burden and resource-limited settings. While microscopy remains useful because of its simplicity, rapid turnaround time, and low cost, its low sensitivity significantly limits its standalone diagnostic value. Culture remains indispensable for definitive confirmation but is constrained by longer turnaround times and higher infrastructure requirements 3, 11.
Limitations
The sample size was modest, which may have affected the precision of sensitivity and specificity estimates. Our future studies with larger cohorts will assess the combined use of GeneXpert, smear microscopy, and culture within diagnostic algorithms to optimize case detection and treatment initiation.
Conclusion
This study reinforces the pivotal role of molecular diagnostics in the modern TB care cascade. While smear microscopy retains utility due to its high positive predictive value and ability to indicate infectiousness, its critically low sensitivity remains a major limitation. In contrast, the Xpert MTB/RIF assay has proven to be a far more reliable tool, offering significantly superior sensitivity and an exceptional ability to rule out disease. Its implementation is indispensable for strengthening TB control efforts, as it facilitates earlier and more accurate diagnosis, enables prompt treatment initiation, and ultimately curbs community transmission.
Therefore, these findings provide robust, local evidence to support the multiple appeals made to national health authorities to equip all TB screening centers across the Republic of Congo with GeneXpert technology.
Authorship contribution statement
FN and DOEA conceived the study. DOEA and MAEN contributed to study design and sample processing or methodology. FHM, JCV, FHOO analysed the data. FN had overall responsibility for the study. AG, FHOO, FHM, and FN were involved in conceptualization, data compilation, editing, and review of drafts, as well as finalization. All authors contributed to drafting the manuscript and read and approved the final version
AI declaration
No AI tools were used for data collection, data analysis, or interpretation of study results.
Funding
This study received financial support from CANTAM (EDCTP-RegNet2015-1045).
Acknowledgements
We thank all participants of this study. We are grateful to the staff of Makelekele Hospital for their support, as well as to the TB Lab CERMEL team for their contributions. FN is a member of CANTAM (EDCTP-RegNet2015-1045). This work was supported by the Central Africa Network on Tuberculosis, HIV/AIDS, and Malaria (CANTAM), funded by the European & Developing Countries Clinical Trials Partnership (EDCTP).
References
- 1.Health World.Organization. (2024).Global tuberculosis report 2024(ISBN 9789240101531). , The Lancet 402(10397), 1845-1846.
- 2.Zumla A, George A, Sharma V, Herbert R H N, Oxley A et al. (2013) WHO’s 2013 global report on tuberculosis: Successes, threats, and opportunities.The Lancet. 382(9907), 1765-1767.
- 3.Somoskovi A, L M Parsons, Salfinger M. (2001) The molecular basis of drug resistance inMycobacterium tuberculosis.Clinical Microbiology Reviews. 14(2), 335-351.
- 4. (2020) World Health Organization.WHO consolidated guidelines on tuberculosis: Module 3: Diagnosis – rapid diagnostics for tuberculosis detection. , Geneva:
- 5.B, J C Djontu, Assiana Elion, O D, F H Mouzinga et al. (2025) Drug-resistant tuberculosis profiles among patients presenting at the antituberculosis center of Brazzaville. , Republic of Congo.Annals of Clinical Microbiology and Antimicrobials 24(1), 31-10.
- 6.Assiana Elion, O D, Abdul J B P A, Linguissi L S G, Epola M et al. (2021) Epidemiological profile of multidrug-resistant and extensively drug-resistantMycobacterium tuberculosisamong Congolese patients.Annals of Clinical Microbiology and Antimicrobials. 20(1), 84-10.
- 7.Zumla A, Nahid P, S T Cole. (2013) Advances in the development of new tuberculosis drugs and treatment regimens.Nature Reviews Drug Discovery. 12(5), 388-404.
- 8.K R Steingart, Henry M, Ng V, P C Hopewell, Ramsay A et al. (2006) Fluorescence versus conventional sputum smear microscopy for tuberculosis: A systematic review.The Lancet Infectious Diseases. 6(9), 570-581.
- 9.C, Nabeta P, Hillemann D, M P Nicol, Shenai S et al. (2010) Rapid molecular detection of tuberculosis and rifampin resistance.The New England. , Journal of Medicine 363(11), 1005-1015.
- 10.K R Steingart, Henry M, Ng V, P C Hopewell, Ramsay A et al. (2006) Fluorescence versus conventional sputum smear microscopy for tuberculosis: A systematic review.The Lancet Infectious Diseases. 6(9), 570-581.
- 11.Becton Dickinson, Company. (2006) . BACTEC™ MGIT™ 960 System user’s manual (Procedure Manual) and Company.https://www.finddx.org/wp-content/uploads/2023/02/20061101_rep_mgit_manual_FV_EN.pdf , Sparks, Maryland, USA: Becton, Dickinson .
- 12.Rimal R, Shrestha D, Adhikari B. (2022) Diagnostic performance of GeneXpert MTB/RIF in detecting Mycobacterium tuberculosis in smear-negative presumptive TB patients. , BMC Infectious Diseases 22(1), 287-10.
- 13.Somoskovi A, Salfinger M, L M Parsons. (2000) culture: Techniques and practical considerations. , Clinical Microbiology Newsletter 22(10), 73-79.
- 14.Houben R M G J, P J Dodd. (2016) The global burden of latent tuberculosis infection: A re-estimation using mathematical modelling. , PLoS Medicine 13(10), 1002152-10.
- 15.Lönnroth K, Jaramillo E, B G Williams, Dye C, Raviglione M. (2010) Drivers of tuberculosis epidemics: The role of risk factors and social determinants. , Social Science & Medicine 68(12), 2240-2246.
- 16.Kissinger P, Manhart L, Papp J. (2018) Clinical presentation and risk factors for tuberculosis. Clinical Infectious Diseases. 66(4), 550-556.
- 17.Rehm J, K D Shield, Joharchi N, P A Shuper. (2009) Alcohol consumption and the global burden of disease. , The Lancet 373(9682), 2223-2233.
- 18.Umair M, M H Rasool, Anwar M. (2020) Comparative evaluation of Xpert MTB/RIF and smear microscopy for diagnosis of tuberculosis. , Journal of Clinical Microbiology 58(2), 01710-19.
- 19.P T Kent, G P Kubica. Centers for Disease Control (1985) Public health mycobacteriology: A guide for the level III laboratory. , Atlanta, GA:
- 20.G K Bunduki. (2018) Evaluation of Xpert MTB/RIF assay for rapid diagnosis of pulmonary tuberculosis in a high-burden setting. , BMC Infectious Diseases 18, 345-10.
- 21.K R Steingart, Henry M, Ng V, P C Hopewell, Ramsay A et al. (2006) Fluorescence versus conventional sputum smear microscopy for tuberculosis: A systematic review. The Lancet Infectious Diseases. 6(9), 570-581.
- 22.K R Steingart, Ramsay A, Pai M. (2007) Optimizing sputum smear microscopy for the diagnosis of pulmonary tuberculosis. Expert Review of Anti-infective Therapy. 5(3), 327-331.
- 23.S D Lawn, Mwaba P, Bates M. (2013) Advances in tuberculosis diagnostics: The Xpert MTB/RIF assay and future prospects. , Clinical Microbiology Reviews 26(4), 669-698.
- 24.World Health Organization. (2011) Automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: Xpert MTB/RIF assay for the diagnosis of pulmonary and extrapulmonary TB in adults and children. , Geneva: WHO.https://www.who.int/publications/i/item/9789241501545
